SARS-CoV-2 Infection Process
In the previous article, Introduction to COVID-19 , we discussed the clinical presentation of COVID-19. In this article, we will explore and learn more about the SARS-CoV-2 (stands for severe acute respiratory syndrome coronavirus 2) infection process. It is important to note that there is a difference between “SARS-CoV-2” and “COVID-19”. SARS-CoV-2 is the virus that causes the disease, COVID-19.
How is SARS-CoV-2 transmitted?
The primary mode of transmission of SARS-CoV-2 is from direct person-to-person contact via respiratory droplets. This means SARS-CoV-2 can be transmitted through methods such as coughing, sneezing, talking, or direct contact with mucous membranes (such as eyes, nose, and mouth). Most public health organizations strongly recommend using face masks and maintaining a physical distance of at least 6 feet between persons. This is recommended because the droplets containing SARS-CoV-2 can land in the mouths or noses of people who are nearby, or they can also be inhaled into the lungs.
SARS-CoV-2 respiratory droplets can also land on surfaces and objects. Studies have shown the virus can remain viable (meaning it may still be able to infect a person) on the surface of some materials for days.
By touching objects and/or surfaces contaminated with SARS-CoV-2, people can become exposed if they then touch their eyes, nose, or mouth after contact with the contaminated surfaces. This is why practicing hand hygiene and frequent surface cleaning can break the chain of infection and prevent SARS-CoV-2 transmission.
Furthermore, there has been growing evidence that SARS-CoV-2 is airborne, so the virus can travel through long distances in enclosed and poorly ventilated spaces and can remain suspended in air for up to a few hours.
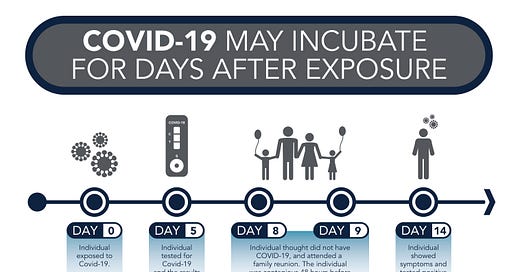
What does the overall timeline look like when a person is exposed to COVID-19?
Once exposed to COVID-19, there is an incubation period (the period between the time of exposure to the symptom onset). This incubation period can last between 1 to 14 days and the symptoms may take up to 14 days to appear after exposure.
It is a common misconception that people are only contagious when they are symptomatic. In reality, studies show transmission can occur up to 3 days before symptom onset.
Furthermore, people who experience mild-to-moderate COVID-19 often remain contagious for up to 10 days after symptom onset. For more severe COVID-19 cases, this timeline can extend past 20 days after symptom onset.
Recovery time depends on the severity of the infection. In mild cases, patients usually recover within one to two weeks. For severe cases, recovery can take up to six weeks or more.
SARS-COV-2 Infection Process
During this pandemic, researchers have been working tirelessly to understand the process of SARS-CoV-2 infection. By figuring out how the virus infects cells, it allows researchers to develop potential treatments to counteract the infection.
The most recent data shows that SARS-CoV-2 infects human cells primarily by binding to a cell surface protein called angiotensin-converting enzyme 2 (ACE2).
ACE2 is a protein on the surface of many cell types. It is most frequently expressed in tissues such as:
● Lungs
● Vasculature (i.e. blood vessels)
● Kidneys
● Heart
● Gastrointestinal tract
ACE2 is involved in a biochemical pathway that is critical to regulating processes such as inflammation, blood pressure, and wound healing.
When the SARS-CoV-2 virus binds to ACE2, ACE2 provides an entry point for the virus to infect human cells. The subsequent cascade of events are shown in the following diagram:
Figure 2: High level overview of SARS-CoV-2 infection process. Adapted from "COVID-19: Pathophysiology and Clinical Findings" by Ryan Brennels. 2020, The Calgary Guide to Understanding Disease. Copyright 2020 by The Calgary Guide.
(Note: This is a high level overview to provide a general picture of the infection process. If you are interested in learning in-depth the scientific details and pathophysiology, please refer to the cited reference above)
By now, you should have a general sense of the SARS-CoV-2 infection process. Stay tuned for the next article to learn more about the different variants of SARS-CoV-2.
References
Brennels, R. (2020). “COVID-19: Pathophysiology and Clinical Findings: Calgary Guide.” Retrieved from https://calgaryguide.ucalgary.ca/covid-19-pathophysiology-and-clinical-findings/
Centers for Disease Control and Prevention. (2021). “COVID-19 Overview and Infection Prevention and Control Priorities in Non-US Healthcare Settings.” Retrieved from
https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/overview/index.html
Centers for Disease Control and Prevention. (2021). ”Ending Isolation and Precautions for People with COVID-19: Interim Guidance.” Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html
Centers for Disease Control and Prevention. (2021). “Science Brief: SARS-CoV-2 and Surface (Fomite) Transmission for Indoor Community Environments.” Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/more/science-and-research/surface-transmission.html
Centers for Disease Control and Prevention. (2021). “Scientific Brief: SARS-CoV-2 Transmission.” Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/sars-cov-2-transmission.html
Government of Canada. (2021). COVID-19 for health professionals: Transmission. Retrieved from https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/transmission.html
Tesini, B. L. (2021). “Coronaviruses and Acute Respiratory Syndromes (MERS and SARS).” Retrieved from https://www.merckmanuals.com/en-ca/professional/infectious-diseases/respiratory-viruses/coronaviruses-and-acute-respiratory-syndromes-mers-and-sars
Trougakos, I. P. et al. (2021). “Insights to SARS-CoV-2 life cycle, pathophysiology, and rationalized treatments that target COVID-19 clinical complications.” Retrieved from https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-020-00703-5