Antibody Mediated Immunity vs Cell Mediated Immunity
In our first article, Immunology 101: Innate and Adaptive Immunity Explained, we briefly introduced the concepts of the humoral immune response and the cell-mediated immune response as components of adaptive immunity. As a quick recall, adaptive immunity (also known as “acquired immunity”, since your body needs to “acquire” or learn to respond to the threat) enables the human body to quickly fight off foreign pathogens (e.g., bacteria, toxins, and viruses) through two main mechanisms: the humoral immune response, primarily driven by B cells, and the cell-mediated immune response, primarily driven by T cells.
These two mechanisms can be quite complex and intricate. Hence, for the purpose of obtaining a general understanding of acquired immunity, this article will contain a simplified and high-level overview of these two mechanisms. A general background knowledge of adaptive immunity will prepare us to discuss an interesting topic: the importance of the humoral immune response in the context of antibody therapies.
1) Humoral Immunity (also known as antibody-mediated Immunity)
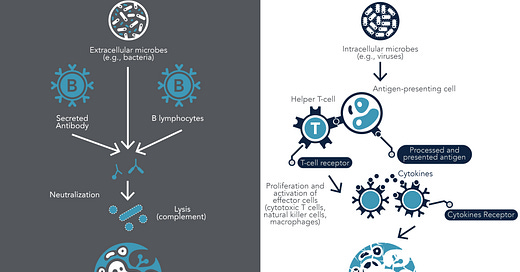
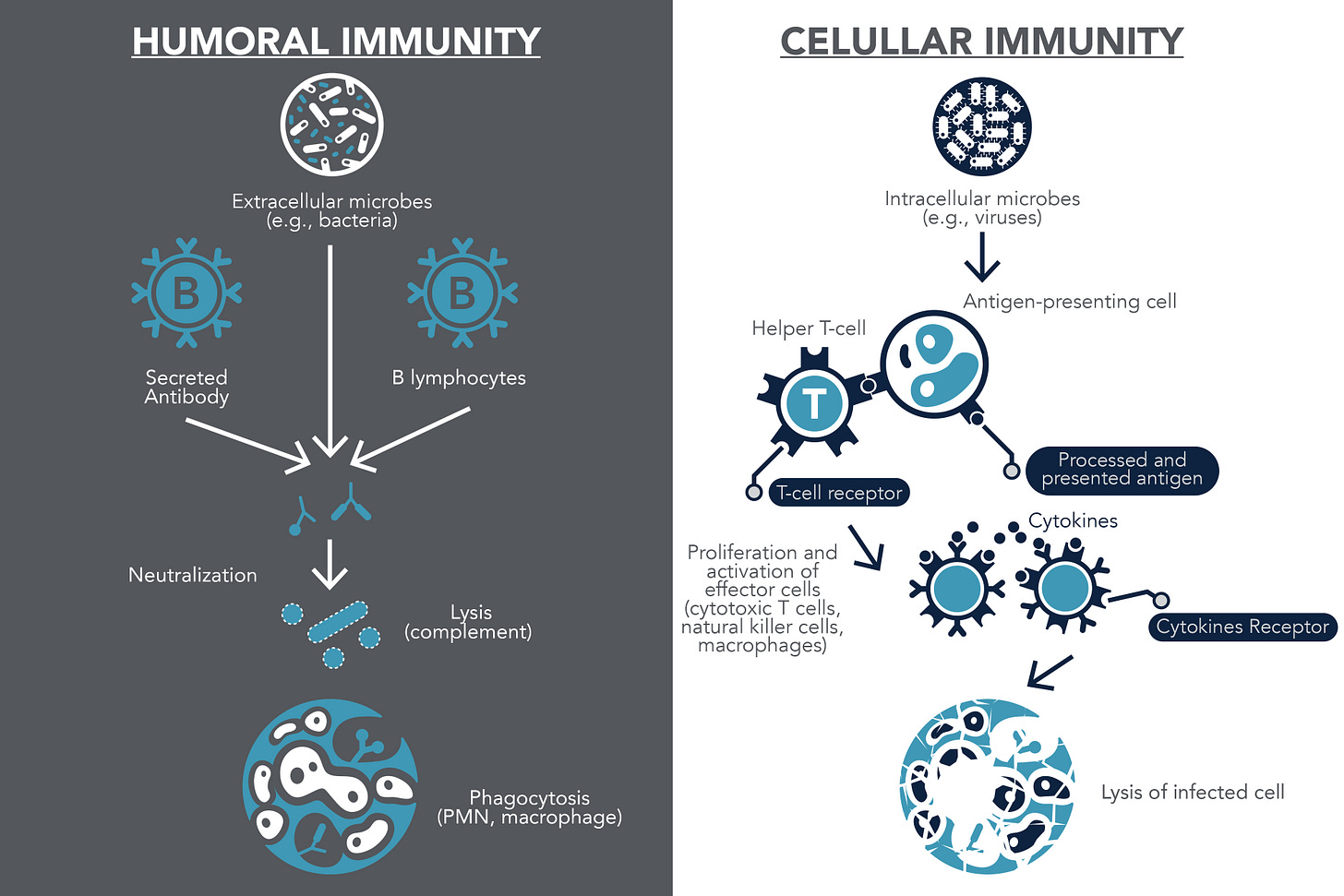
Antibody-mediated immunity occurs when an antigen of a foreign pathogen is detected in the human body. This mechanism is primarily driven by B cells (also known as B lymphocytes), which are activated to produce and secrete antibodies after detecting a specific antigen. These secreted antibodies are important to prevent infection before it happens, and can also target (or “label”) these threats or infected cells for destruction.
B cells are very specific, with each B cell recognizing a specific antigen. Naive B cells are B cells circulating in the body that have never encountered their matching antigen and these B cells travel throughout the body looking for their target. When naive B cells find their matching antigen, they undergo a process known as differentiation, which leads to the production of antigen-specific plasma cells and memory B cells.
Plasma cells produce antibodies with antigen-specific binding sites into the blood stream. These antibodies now circulate in the body and bind the pathogens that have the matching antigen on their surface. When bound, these antibodies can fight off the pathogen through the following mechanisms:
Deactivate (or neutralize) the pathogen
Bind and signal innate immune cells (e.g., macrophages) to engulf and ingest the foreign cells (this mechanism is also known as “phagocytosis”)
Activate the complement system which induces a series of inflammatory responses and “complements” the ability of the immune system to attack pathogen
Like its name implies, memory B cells will “memorize” the foreign antigen for the future. Thus, when the same antigen is seen in the body again, the memory B cell will produce antibodies quickly (faster than the first time) to get rid of the infection (refer to Figure 1).
2) Cell-mediated Immunity
In contrast to humoral immunity, cell-mediated immunity does not rely on antibodies to respond to threats. Cell-mediated immunity also cannot respond to threats that exist outside of the cell, like an antibody does when it blocks infection. Instead, cell-mediated immunity is important in targeting threats that exist within a cell, for instance, a cell that is already infected by a virus or a cancerous cell. Cell-mediated immunity is primarily driven by T cells.
The two main types of T cells are helper T cells (also known as CD4 T cells) and cytotoxic T cells (also known as CD8 T cells) and they bind to Major Histocompatibility Complex (MHC) class II proteins and MHC I proteins, respectively.
What are Major Histocompatibility Complex (MHC) proteins? MHC play a critical role in cell-mediated immunity because they present the antigen (from the pathogen) onto the cell surface for T cell recognition.
MHC class I proteins are expressed on the cell surface of most cells in the human body (except red blood cells).If a cell is infected with a pathogen (e.g., virus), the cell will present the peptide antigen (from the pathogen) on the cell surface via MHC class I protein, which then marks it for destruction. Subsequently, this will be presented to the cytotoxic T cells which kills the infected/cancerous cell. This is a critical mechanism in our body because the elimination of infected body cells will prevent the replication of pathogens and cancer cells in the human body.
MHC class II proteins are expressed on the cell surface of professional antigen presenting cells (e.g., macrophages). When an antigen presenting cell engulfs a pathogen, it will present the peptide antigen (from the pathogen) on the cell surface via MHC class II protein. This will then be presented to the helper T cells, which release cytokines (inflammatory cells) that act like “alarm bells” to activate effector cells (e.g., cytotoxic cells, natural killer cells).
Similar to antibody-mediated response, cell-mediated response has memory T cells that will “memorize” this event and react quickly if the body encounters the same pathogen again (refer to Figure 1).
How does antibody-mediated immunity relate to antibody therapy research?
Let's start off with a real-life example:
Smallpox is a very contagious and deadly disease with a 30% fatality rate. Potential complications of smallpox include permanent skin scarring (especially on the face, legs and arms) and blindness.
Thanks to the research conducted by an English physician Dr. Edward Jenner (1749–1823), a smallpox vaccine was developed, and the World Health Organization announced the world free of smallpox on May 8, 1980.
Vaccines are developed by taking advantage of the antibody-mediated response in the human body.
One can acquire antibody-mediated immunity to a specific infection or disease when:
administered with antibodies from another host who has previously been exposed to the same pathogen
administered a weakened (non-dangerous) version of the pathogen (or a species similar to it) which triggers the immune system to develop specific antibodies
In the case of smallpox, the current vaccine contains the vaccinia virus, which is a type of virus similar to variola virus (smallpox is caused by the variola virus) but it is less harmful. Once this vaccine is administered to a patient, the antibody-mediated response system will produce specific antibodies and memory B cells. As a result, if the vaccinated patient is exposed to smallpox, memory B cells can quickly produce specific antibodies that can fight off the smallpox.
So why do we need vaccines if we already have our immune system to protect us? As you can see from the smallpox case, our natural immune system may not be able to provide 100% protection from all diseases. Various factors can affect our natural ability to fight off diseases. For example, as we age, our immune system becomes weaker and it becomes slower to respond to foreign invaders. Thus, vaccines play a key role in complementing our immune system, providing us the protection to prevent deadly diseases and to prevent potentially severe complications (as exemplified from the smallpox case we discussed above).
As you can see, by leveraging the mechanism of antibody-mediated response, researchers can develop vaccines, antibody therapies or improve current lines of therapy to address the gaps in available treatment for various infections and diseases.
References:
Alberts B, Johnson A, Lewis J, et al. (2002). Molecular Biology of the Cell. New York: Garland Science.
Centers for Disease Control and Prevention. Vaccine Basics. (2017). Retrieved from https://www.cdc.gov/smallpox/vaccine-basics/index.html
Centers for Disease Control and Prevention. (2021). History of Smallpox. Retrieved from https://www.cdc.gov/smallpox/history/history.html
Center for Biologics Evaluation and Research. (2018). ACAM2000 (Smallpox Vaccine) Questions and Answers. Retrieved from https://www.fda.gov/vaccines-blood-biologics/vaccines/acam2000-smallpox-vaccine-questions-and-answers
Delves, P. J. (2020). Overview of the Immune System - Immune Disorders. Retrieved from https://www.merckmanuals.com/en-ca/home/immune-disorders/biology-of-the-immune-system/overview-of-the-immune-system
Dornell, J. (2021). Humoral vs Cell-Mediated Immunity. Retrieved from https://www.technologynetworks.com/immunology/articles/humoral-vs-cell-mediated-immunity-344829
Hewitt, E. W. (2003). The MHC class I antigen presentation pathway: Strategies for viral immune evasion. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1783040/
Janeway CA Jr, Travers P, Walport M, et al. (2001) Immunobiology: The Immune System in Health and Disease. 5th edition. New York: Garland Science; 2001. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK10762
Kisielow, P. (2019). How does the immune system learn to distinguish between good and evil? The first definitive studies of T cell central tolerance and positive selection. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6790186/
World Health Organization. (2020). How do vaccines work? Retrieved from https://www.who.int/news-room/feature-stories/detail/how-do-vaccines-work
World Health Organization. (2020). Smallpox. Retrieved from https://www.who.int/news-room/q-a-detail/smallpox